Dr. Witherspoon: Get it right
Published 10:17 am Friday, February 16, 2024
|
Getting your Trinity Audio player ready...
|
One must remain on the cutting edge.
There was a new technique available for removing the gallbladder. They could now remove it using a thin fiber-optic scope, leaving practically no scar.
A woman who needed her gallbladder removed was offered this new technique and enthusiastically agreed.
Postoperatively, she was nauseated, unable to eat and had severe abdominal pain.
Tests revealed the surgeon had accidentally cut the common bile duct. He took her back to the operating room, opened her abdomen and repaired it.
It was determined that the doctor was likely inadequately trained to do the operation. He had taken a two-day course on how to use the laparoscope, assisted another doctor on several cases, then began operating on his own.
She was his first case.
Dr. Witherspoon says:
This is nothing more than a lack o’ plain ol’ common sense. There you are in the middle of an operation, patient’s asleep, incision’s made, and you come to the brilliant conclusion you don’t know what you’re doing because you’ve never done it before!
When the laparoscopic gallbladder technique first came out, it was quickly recognized as one of the major advances in modern medicine. As soon as they could get their hands on the equipment, surgeons rushed to the OR fearing they’d be left behind.
And many promptly blew it.
Doctors who were trained to open the abdomen and operate with their hands found themselves struggling with these danged little sticks, grabbing for things they couldn’t feel, heads turned sideways at the t.v. screen, trying to figure out what they were looking at. It could be frustrating to no end, like trying to teach grampaw to eat his peas with chopsticks. If you saw drops dripping up and bubbles floating down, it could suddenly dawn on you — you’re operating upside down!
The complication rate was astounding. They cut the bowel, cut the common bile duct, shredded the liver — if it was in the abdomen, somebody nailed it with the scope. Even the aorta got whacked. Malpractice insurance companies were beside themselves. One insurance company put together a training course and offered surgeons a discount on their premiums if they attended it. The only purpose of the course was to show them how not to cut the common bile duct while taking the gallbladder out with the scope.
An article in the New York Times bemoaned the “rising number of deaths and serious injuries from a new method of gallbladder surgery.” The New York Health Department insisted a surgeon’s first fifteen laparoscopic gallbladder cases be performed under supervision, complaining that “…a learning curve was not justification for serious injury to patients.” It was suggested surgeons offer their first few patients a discount to compensate for the increased risk.
After the dust had settled from all the injuries, we learned the complication rate is ten times higher during the first 6 or 7 cases if done unsupervised, compared to all others done thereafter. The technique requires a learning curve, folks. And watching somebody else doesn’t count. You can’t learn baseball from the stands — you gotta get out there and pitch. Likewise, the doctor learning the technique should be the primary surgeon operating under the guidance of an experienced proctor, not just an assistant. That won’t cut it. You have to do it yourself. The supervisory surgeon can step in and take over if you get in trouble, so the arrangement is safe. Do a few like that and you’re good to go.
Did we learn a little lesson here?
Apparently not. Some years later, orthopedics was inundated with runaway enthusiasm for minimally invasive total joint replacements. Do ‘em through tiny incisions and patients will walk out the next day after hip replacement surgery loving it. Equipment reps were telling orthopods they were gonna get buried if they didn’t hurry up and do it the new way.
Then the lead article in a premier orthopedic journal decried the high complication rate associated with minimally invasive hip replacements due to inadequate training. They put the components in wrong: sideways or whatever. Patients had recurrent dislocations, loose components and some got infected. They had to be taken back to the OR to go through it all over again to get it done right.
Some years later we experienced the same for the direct anterior approach for hip replacements. Studies demonstrated a high complication rate during the surgeon’s first 15 to 30 cases. Same for the robot.
It all comes down to proper training and, for some reason, we consistently neglect that.
The two culprits that get us into trouble are the rush to get onboard with a new procedure, usually with serious goading by administration who perennially has dollar signs in their eyes, and the surgeon’s never-ending over-estimation of his abilities. Drives me nuts.
Obviously, the responsible thing to do is develop a standard training regimen for new procedures, require surgeons to satisfy the criteria before going solo, and get every hospital onboard. Seems ridiculously simple to me but, presently, there is no standardization.
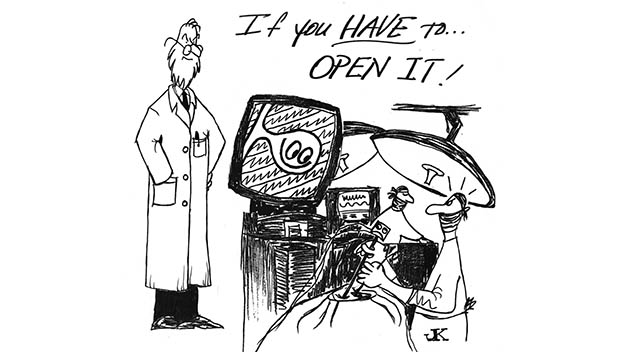
Final point. The most common cause of injury with the gallbladder operation was failure to resort to the old-fashioned method when the surgeon was hopelessly fouled up with the scope. To keep pluggin’ away at it when you don’t know what you’re doing is extremely dangerous. That’s when bad things happen. If you promised your patient a cute little scar you can cover with a Band-Aid, you could be in trouble.
You have to know when to call it quits and do it the old way. Have a “plan B,” as one neurosurgeon put it. The patient must accept that possibility and it must be documented before you cut skin.
Goes in the pre-op note.
Informed consent ‘n’ reasonable expectations – words for surgeons to live by.
J. M. MacDavid M.D. also known locally as Dr. John Kona can be contacted at WitherspoonInstitute23@gmail.com.